Beyond chemotherapy: Navigating the promise and perils of CAR-T therapy in pediatric cancer
However, cancer treatment has evolved significantly over the last few decades.
Opie's journey
For Opie Jones, who was diagnosed with an acute case of leukaemia at five months old, CAR-T therapy became his last option, after multiple rounds of gruelling chemotherapy and a bone marrow transplant failed to eliminate his cancer.
Opie became the ninth baby in Europe to receive his own modified T-cells at Great Ormond Street Hospital in London. The novel treatment was successful and Opie, now aged three, remains cancer-free.
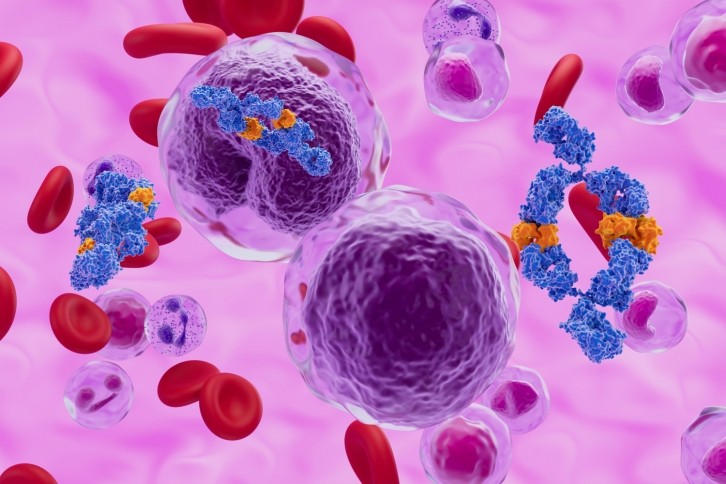
CAR-T therapy, a relatively new concept in oncology treatment, involves extracting T-cells from a patient’s blood and reprogramming them to target and kill the cancer cells.
In the UK, CAR-T therapy is currently available for children under 25 months who have had relapsed acute lymphoblastic leukaemia (ALL).
After hearing her son would be receiving CAR-T, Lucy Ellerker came across the Emily Whitehead Foundation – named after the first child to receive the highly experimental treatment in a clinical trial and be successfully treated back in 2012.
After he achieved remission, Lucy and her husband, Lewis Jones, decided to set up a charity dedicated to her son – called The Opie Jones Foundation – providing mental health support to families going through their childhood cancer experiences, advocating for CAR-T therapy, and pushing for wider adoption.
“I want to bring hope. My husband and I would lift each other up. If one of us was down, the other was doing ok. We’d balance our emotions. But we would always have hope and CAR-T gave us the biggest hope that Opie was going to survive and we’d get to take our baby home. I want to share that with other families and give them that same hope,” she says.
Advocacy for CAR-T
Now, Lucy is focused on championing CAR-T therapy and spreading Opie’s story as ‘far and wide as possible’ as she admits ‘running a charity is much more than I ever imagined it to be’.
At Advanced Therapies Lisbon 2023, George Eastwood, executive director of the Emily Whitehead Foundation also announced that the organization would be donating $10,000 to the newly formed Opie Jones Foundation.
“To have the Emily Whitehead foundation with George and Tom helping us and collaborating with us – strengthens us.” Lucy adds.
After watching her child suffer from the side effects of chemotherapy, Lucy believes that CAR-T therapy should be offered as a first treatment option, rather than only being available after a child’s cancer returns – as the current National Institute for Health and Care Excellence (NICE) regulations state.
“Knowing what we know now, the question is – why couldn’t we have had that first? I firmly believe that if Opie had been able to have CAR-T first, he may not have needed to have all the toxic treatments that made him incredibly sick” she says.
When giving talks and presentations, Lucy shares a picture of Opie a week after his bone marrow transplant and a week after CAR-T therapy.
“The thing that stands out the most – after his bone marrow transplant – he looks like a kid with cancer. He has no hair, no eyebrows and has his feeding tube in – he looks poorly,” she adds.
“The picture after CAR-T – he’s got all this lovely blonde hair that eventually came back, he didn't lose that. He had his feeding tube for maybe a few days, but he didn't really need it, because his body wasn't having to recover as much from such a severe treatment.”
Lucy also describes the process of getting a bone marrow transplant as incredibly time-consuming and fraught with anxiety.
“We had to wait for a donor. The donor cells then needed to be harvested and his cells came from America – that all takes time. In that time, his leukemia was getting worse.
“The conditioning treatment for the bone marrow transplant itself was also a lot harsher because they had to effectively empty his bone marrow to make room for all the new cells that are going to take over when the new donor cells can graft. However, with CAR-T, they’re just making a bit of room for it. That’s how I understand it,” she says.
Challenges and controversies
So, despite its achievements and promise, why hasn’t CAR-T therapy been rolled out as the first point of call for pediatric cancer care?
A major factor is cost, with Brian Koffman, founder of the Chronic Lymphocytic Leukemia Society, saying CAR-T is the ‘most expensive Medicare diagnosis-related drug’. While access to the therapy has improved as it has progressed, it has remained expensive to run.
However, George argues that it is important to look at the overall value and bigger picture, arguing that ‘the headline is always how expensive it is rather than how brilliant and curative it is’.
“One point that Emily Whitehead’s father Tom often makes – is that it cost over $2 million to his Medicare to not cure Emily over those 22 months of treatment. Although Emily was part of a clinical trial and there was no payment, Kymriah, the therapy she received was $473,000 – so the value is a mess,” he says.
“Somehow, we’re quick to vilify pharma for charging $473,000. But we don't vilify our hospitals for charging $2 million. It's broken up better so it's not this lump sum charge.”
Another concern is the neurological side effects of CAR-T therapy, such as speech problems, delirium and seizures, which can be severe or fatal.
“The neurological risk happens when the T cells are released back into the body. The immune response is so massive, it causes something called Cytokine release syndrome, which is this neurologic response. It happened with Emily because she was the first patient. She was in intensive care,” George says.
In response, the Emily Whitehead Foundation has funded a study investigating the neurocognitive effects of CAR-T with a doctor that is following up with many patients in remission who received the therapy at the University of Pennsylvania.
“By sharing this data and seeing great results from these studies, we hope it will instil confidence and provide the information need,” George says.
“The notion that CAR-T could cause neurological effects was devastating to me. However, chemotherapy and radiation also pose serious neurocognitive risks. This data could come out and CAR-T may be a lot better. It’s certainly not game over."
In order for CAR-T to be moved further up the line, rather than administered as a last resort, there must be ‘accumulation of more data’ and ‘the right studies’ as well as strong parents like Lucy to push that forward and ensure progress is happening, he adds.
“We need more education. When I was back at the hospital with Opie, there were some nurses and doctors who said – tell me more about CAR-T? And you think – you work in oncology? It’s mind-blowing and it’s working out how to join the dots together to break down these barriers,” she says.
“In the UK we have the NHS which is an amazing healthcare service to have. But financially, they would need to spend a lot of money to catch up with how technology is moving forward as well as amazing scientific advances coming in.”
For Lucy, it is important than pediatric cancer treatment continues to evolve and the toxic effects of chemotherapy are acknowledged – with more attention and investment towards burgeoning options like CAR-T therapy.